REBYOTA has confirmed >90% coverage for commercially and government-insured patients.* Learn More
Access information and support tools for REBYOTA
including coding, billing, coverage, reimbursement, and financial assistance.

REBYOTA CODING AND BILLING
Table of Codes
Enterocolitis due to Clostridium difficile, recurrent
Enterocolitis due to Clostridium difficile, not specified as recurrent
(accepted by most payers)


Fecal microbiota, live – jslm, 1 mL billed as 150 mL
- Hospital Outpatient includes pass-through status
- For Ambulatory Surgical Center (ASC) Medicare Fee-For-Service (FFS)
please see below for product coverage informationa
MEDICARE FEE-FOR-SERVICES (FFS) WHEN BILLING AS:
Instillation of fecal microbiota suspension
XW0H7X8
Introduction of broad consortium microbiota-based live biotherapeutic suspension into lower GIc
Instillation of fecal microbiota suspension
COMMERCIAL/MEDICAID/MEDICARE ADVANTAGE
Instillation of fecal microbiota suspension
Instillation of fecal microbiota suspension
aMedicare makes separate payment to ASCs for certain covered ancillary services that are provided integral to a covered ASC surgical procedure. REBYOTA J1440 is listed on the Medicare ASC fee schedule. 0780T is currently NOT listed as a covered procedure for ASCs with a published fee schedule and therefore J1440 may not be reimbursed in ASC setting. These procedures can be found on the ASC addendum AA at medicare/medicare-fee-for-service-payment/ascpayment/11_addenda_updates.
cHospitals can report this code on forms related to REBYOTA to receive the add-on payment for eligible inpatient cases, when applicable.
dSkilled Nursing Facility (SNF), Long-Term Acute Care (LTAC), etc.
Disclaimer: 1. The reimbursement information provided by Ferring is intended to provide general information relevant to coding and reimbursement of Ferring products only. Coverage and payment policies for the same insurer, such as Medicare, can vary from one region to another and may change from time to time because of ongoing changes in government and insurance industry rules and regulations. Please confirm HCPCS codes with the Pricing, Data Analysis and Coding (PDAC) contractor or your local DME MAC before processing claims. Ferring does not guarantee coverage or payment of its products. 2. These potential codes are provided for informational purposes only. Providers must use their independent judgment to select the codes that most appropriately describe the items or services provided to a patient. Providers are responsible for compliance with Medicare and other payer rules and requirements and for the information submitted with all claims and appeals. Providers should review applicable payer instructions and requirements and confirm the accuracy of their coding or billing practices with payers before claims or appeals are submitted.
REBYOTA SUPPORT FOR PROVIDERS
Summary of Services Offered Through REBYOTA Connect
Access and
Reimbursement
Services
- Benefits investigation
- Prior authorization (PA) information
- Appeals assistance for PA or claim denials
- Billing and coding support
Co-pay Support
Program
Screen patients for eligibility for co-pay support and, if eligible, initiate enrollment in the REBYOTA co-pay program.
Patient Assistance
Program
Screen patients for eligibility into the patient assistance program which provides REBYOTA at no cost to eligible patients. Assistance for eligible patients will be provided in the form of free product shipped to site of administration or reimbursement for the purchase price of the product if processed after product administration.
Patient
Education
Refer patients to REBYOTA educational materials, C. difficile support groups, and/or state health exchanges if they are uninsured.
For help in verifying a patient’s insurance coverage…
call REBYOTA CONNECT at 1-877-REBYOTA (1-877-732-9682) or to begin enrollment, visit REBYOTACONNECT.COM
REBYOTA CONNECT
Enrollment Form
REBYOTA CONNECT Hub
Enrollment Instructions
and Checklist
TIPS FOR DETERMINING PATIENT BENEFITS WITHOUT THE HELP OF REBYOTA CONNECT
The accurate completion of coverage-related documentation is the responsibility of the healthcare provider and patient.
Consider using the checklist below to help verify the patient’s insurance coverage:
- Ask if the patient has coverage through Medicare, Medicaid, or private insurance
- Ask to see the patient’s insurance card
- Contact the patient’s insurance plan to determine coverage
- Check for coverage under both medical benefit and pharmacy benefit
- A prior authorization (PA) may be needed. If that is the case, the following may be helpful:
A Patient Assistance Program
is available for patients who are uninsured
or underinsured and need financial assistance.
Ensure you complete section 3 of the enrollment form.
REBYOTA SUPPORT FOR PATIENTS
CO-PAY ASSISTANCE PROGRAM
Eligible, commercially insured patients may pay as little as $100 of their co-pay, coinsurance, or deductible.
Visit www.HCP.REBYOTACopay.com for more details. Terms and conditions apply.
PATIENT ASSISTANCE PROGRAM
Drug Program for uninsured/underinsured patients who meet eligibility criteria.
Visit www.REBYOTACONNECT.com for more details. Terms and conditions apply.
Reimbursement
Understand REBYOTA product reimbursement for Medicare, Medicaid, and private payers (commercial insurance).
Downloadable Forms
Use these resources to streamline access to REBYOTA for your patients with recurrent C. difficile infection.

Sample Appeals Letter
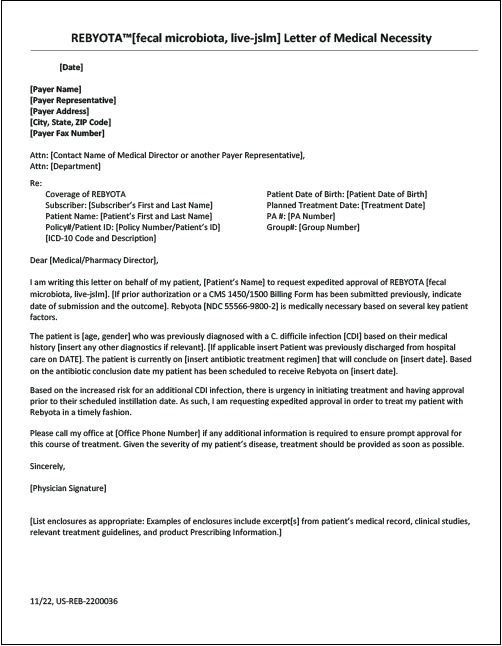
Sample Letter of Medical Necessity

Sample CMS 1450 Billing Form
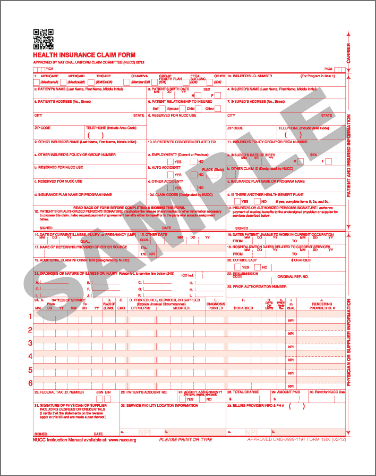
Sample CMS 1500 Billing Form
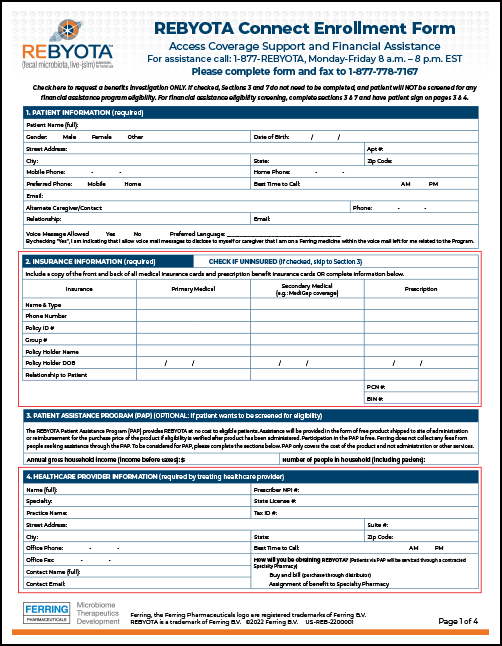
REBYOTA CONNECT Enrollment Form
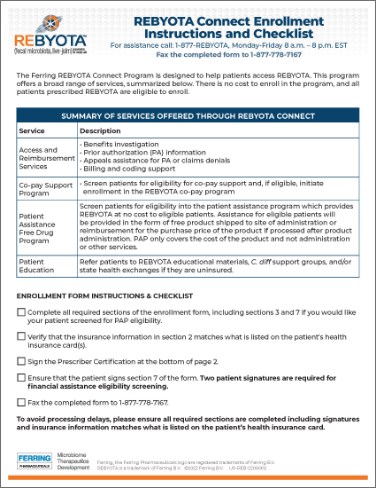
REBYOTA CONNECT Hub Enrollment Instructions and Checklist
REBYOTA Coding, Coverage, and Reimbursement Guide
Ordering Instructions
There are multiple ways to order REBYOTA: through major specialty distributors, REBYOTA @ Home, or specialty pharmacies.
Why Rebyota
Answers to REBYOTA questions including administration, safety, patient expectations, and more.
Sign up to receive information
and updates on REBYOTA
IMPORTANT SAFETY INFORMATION
INDICATION
REBYOTA (fecal microbiota, live – jslm) is indicated for the prevention of recurrence of Clostridioides difficile infection (CDI) in individuals 18 years of age and older, following antibiotic treatment for recurrent CDI.
Limitation of Use
REBYOTA is not indicated for treatment of CDI.
IMPORTANT SAFETY INFORMATION
Contraindications
Do not administer REBYOTA to individuals with a history of a severe allergic reaction (eg, anaphylaxis) to any of the known product components.
Warnings and Precautions
Transmissible infectious agents
Because REBYOTA is manufactured from human fecal matter, it may carry a risk of transmitting infectious agents. Any infection suspected by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to Ferring Pharmaceuticals Inc.
Management of acute allergic reactions
Appropriate medical treatment must be immediately available in the event an acute anaphylactic reaction occurs following administration of REBYOTA.
Potential presence of food allergens
REBYOTA is manufactured from human fecal material and may contain food allergens. The potential for REBYOTA to cause adverse reactions due to food allergens is unknown.
Adverse Reactions
The most commonly reported (≥3%) adverse reactions occurring in adults following a single dose of REBYOTA were abdominal pain (8.9%), diarrhea (7.2%), abdominal distention (3.9%), flatulence (3.3%), and nausea (3.3%).
Use in Specific Populations
Pediatric Use
Safety and efficacy of REBYOTA in patients below 18 years of age have not been established.
Geriatric Use
Of the 978 adults who received REBYOTA, 48.8% were 65 years of age and over (n=477), and 25.7% were 75 years of age and over (n=251). Data from clinical studies of REBYOTA are not sufficient to determine if adults 65 years of age and older respond differently than younger adults.
You are encouraged to report negative side effects of prescription drugs to FDA. Visit www.FDA.gov/medwatch, or call
1-800-332-1088.
Please click here for full Prescribing Information.
References
- Medicare Claims Processing Manual. Chapter 17—Drugs and Biologicals. https://www.cms.gov/regulations-and-guidance/guidance/manuals/downloads/clm104c17.pdf. Accessed July 14, 2022.
- Medicaid Covered Outpatient Prescription Drug Reimbursement Information by State. https://www.medicaid.gov/medicaid/prescription-drugs/state-prescription-drug-resources/medicaid-covered-outpatient-prescription-drug-reimbursement-information-state/index.html. Accessed July 14, 2022.
- Provider payment and delivery systems. Medicaid 101. https://www.macpac.gov/medicaid-101/provider-payment-and-delivery-systems. Accessed November 30, 2022.







